COVID-19 and Spinal Cord Injury
Coronavirus and SCI
This information was updated February 2023. Please check the Centers for Disease Control and Prevention (CDC) website for breaking and updated information.
A new virus was discovered in 2019. Since it is unique and not previously existing, it is called a novel virus. This specific virus strain, although new, does belong to a family of viruses called SARS (Severe Acute Respiratory Syndrome.) In February 2003, SARS-CoV (Severe Acute Respiratory Syndrome-associated COrona Virus) spread throughout the world. It later became known by the shortened version SARS.
COVID-19 is the abbreviated name for COrona (CO) VIrus (VI) Disease (D) discovered in 2019 or COVID-19. COVID-19 is like other viruses. A virus has one purpose in its life and that is to survive. It will multiply and mutate (alter its structure) to keep living. They change forms to stay alive. Therefore, viruses can be hard to treat. People who have a virus are contagious because that virus wants to spread to keep alive.
Viruses behave in a certain way. They are extremely tiny which makes it easier to enter the cells of your body. A virus is not a cell, but protein surrounded by a spiky outer skin called an envelope. Once inside a body cell, the virus will replace the natural cell duplication process with the virus’s duplication process. The cell no longer reproduces itself but instead reproduces the virus. It can then travel throughout the body so the virus can spread easily and quickly within us. Viruses have no cure but rather vaccines are developed that either destroy the virus in the body or prevent the virus from entering the cell.
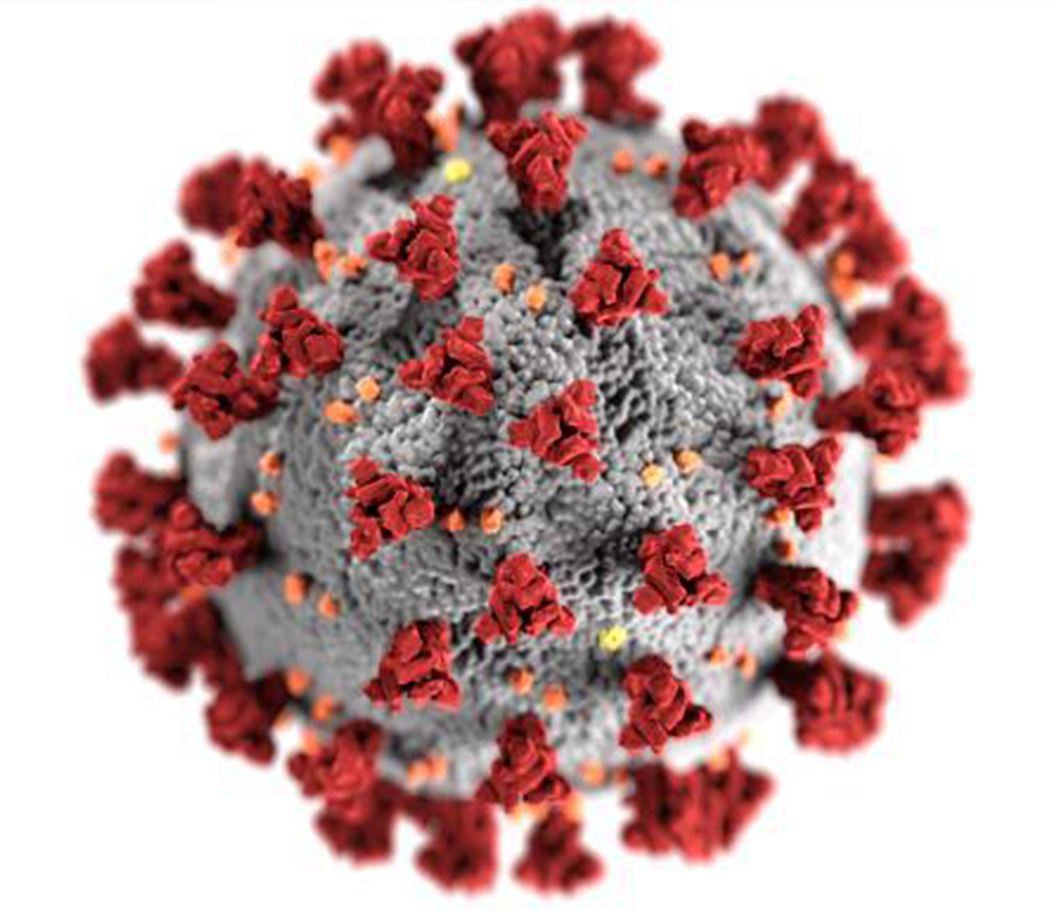 The name given to this 2019 virus is Corona because when you see the virus under a microscope, its spiky surface looks like thorns in a crown (corona in Latin) because the spike protein attaches itself to human cells to infect those cells the spike proteins are essential for COVID-19.
The name given to this 2019 virus is Corona because when you see the virus under a microscope, its spiky surface looks like thorns in a crown (corona in Latin) because the spike protein attaches itself to human cells to infect those cells the spike proteins are essential for COVID-19.
The COVID-19 virus spreads rapidly. It is transmitted from person to person by droplets from your respiratory system through coughing and saliva from an infected person, to the mucous membranes of another person. Mucous membranes are moist openings such as your eye, nostrils, mouth, genitals or rectum. It can float around in air currents to reach from one person to another, live on surfaces that are later touched, through direct contact like touching, kissing, speaking , breathe, cough other physical contact.
When you connect with the contaminated droplet either by breathing in or by touching the virus to a mucous membrane, entry into your body occurs. Individuals who contract COVID-19 have a significant variety in the course of their illness. Some individuals are asymptomatic (have no symptoms), non-severe symptomatic (manage their symptoms at home), or severe respiratory and systemic presentations (hospitalization or intensive care treatment is required). It is estimated that over 90% of individuals who have COVID-19 recover without advanced medical care.
What Happens when COVID-19 Enters the Body
Mucous membranes, the moist surfaces at the openings of your body will provide an entry for COVID-19. If a droplet of COVID-19 enters your body, it favors the respiratory system because there are many ACE-2 (angiotensin-converting enzyme 2) receptors on cells. The ACE-2 receptors are proteins that allow COVID-19 easy access into your cells. The spike of the COVID-19 virus attaches to the ACE-2 receptor and enters the body cell. There are many ACE-2 receptors deep within your lungs which is why COVID-19 affects breathing so severely. Also, because there are ACE-2 receptors elsewhere in the body COVID-19 can affect the arteries, heart, kidneys and intestines.
COVID-19 affects the body by activating the immune system which is controlled by the Autonomic Nervous System (ANS). The immune system is the part of the body that responds to bacteria, viruses, parasites and fungi. Viruses are perceived by the body’s immune system through infection-fighting substances including white blood cells and cytokines, natural small proteins that travel around in the blood and prevent viruses from entering the body’s cells. They signal the brain through the ANS that detection of an invader or pathogen is present.
The ANS directs the body to produce natural antibodies which are proteins produced by white blood cells to capture and rid the body of pathogens when they are detected. Natural antibodies are made by your body. Often, this extra boost of antibodies is needed to help fight an infection quickly and efficiently.
If the virus multiplies too quickly for the ANS to stop it, the infection spreads. The ANS can be affected by spinal cord injury (SCI) by causing a slow response to detect infection or a slow ability to produce natural antibodies to control it. COVID-19 is a virus that affects the respiratory system, but the virus will continue to duplicate throughout the body, affecting all major organs especially if the ANS cannot respond effectively or quickly. In those affected by spinal cord injury, there is a higher risk of entry through the urethra or rectum while doing personal care.
Other important organs of the immune system are the lymph system and spleen. The lymph system is the main removal section of the immune system. Lymph nodes are located throughout your body. They trap any foreign invader in the body and neutralize it by using white blood cells, particularly those called leukocytes. Leukocytes are produced in your bone marrow. When you have an infection, you might notice a lump nearby the area of concern. This is probably a swollen lymph node doing what it needs to do which is to kill whatever is harmful to your body.
The spleen is under the ribs, below the lung on the left side of your body. The spleen filters your blood to destroy foreign material. It also stores the patterns for natural antibodies until they are needed. Once a pathogen has been documented within the body, the spleen stores the information to be used should that pathogen reappear.
In COVID-19 as with other rapidly spreading infections, there is an imbalance in the immune system especially in the depletion of T cells (pathogen fighters) and the production of too many cytokines. This produces a ‘cytokine storm’ syndrome (CSS) or far too many cytokines in the body at once. Cytokines work to help rid the body of infection but in CSS, too many cytokines are made which start to destroy healthy tissue as well. This cytokine storm develops in the most severe and fatal cases of COVID-19.
Some effects of COVID-19 in the body include changes in the respiratory system but also: Cytokine storm syndrome (CSS), continuous or intermittent fever for extended periods of time, cough, difficulty breathing, severe body aches, dizziness, headache, reduced consciousness, acute cerebrovascular disease including stroke, loss of control of body movements, seizures, alterations in the peripheral nervous system (PNS), loss of taste and smell, small vessel blood clots or embolus in the bowel, vascular changes throughout the body, discolored toes and/or fingers known as COVID toe, and multisystem inflammatory syndrome in children (MIS-C). These changes have been noted to be temporary as well as with long-term consequences.
Symptoms of COVID-19
Symptoms of COVID-19 appear 2-14 days after exposure to the virus. You can be contagious with COVID-19 before symptoms appear or perhaps, even without ever having symptoms. Most individuals who have COVID-19 will have a fever of 100.5°. The list of COVID-19 symptoms is evolving but includes:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Risk Factors for COVID-19
Everyone has an equal chance of getting COVID-19 if exposed. There are risk factors that can affect the severity of the virus’ course. You can have no risk factors and still have a severe case. Individuals with multiple risk factors have had mild cases. However, individuals with risk factors do tend to have more severe cases. Risk factors include:
Age The risk of contracting COVID-19 in younger age groups is advancing. Thought to increase risk in children are medical conditions including but not limited to: obesity, medical complexity, severe genetic disorders, severe neurologic disorders, inherited metabolic disorders, congenital (since birth) heart disease, diabetes, asthma and other chronic lung disease, and immunosuppression due to malignancy or immune-weakening medications.
A rare complication of COVID-19 in children is Multisystem Inflammatory Syndrome in Children (MIS-C), a serious condition that inflames various parts of the body. Symptoms of MIS-C include fever and either some or all these symptoms: abdominal (gut) pain, vomiting, diarrhea, neck pain, rash, bloodshot eyes, or feeling extra tired. The cause of MIS-C is currently unknown.
Young adults can contract COVID-19 the same as individuals of any age. Those with more severe cases tend to have these risk factors: obesity or overweight, asthma, smoking, vaping, or a history of smoking and/or vaping.
Older adults aged 65 and greater appear to have more severe cases with severity increasing with age. This is probably due to a slowing of the immune system. As a normal part of aging, the development of T cells that fight infection become less effective.
Race/ethnicity Genetically, humans are the same. Race does not affect COVID-19 however, the cultural, social, economic, education and ritualistic values of a group of people can affect COVID-19 risk. Black, Latino, American Indian and Alaskan Native people are hospitalized for COVID-19 in higher proportion than the general population. Most classification systems hold on to the archaic use of race as a differentiation for assessment purposes.
Gender Men are more often affected with poorer outcomes from COVID-19 than women. There are a variety of suggested reasons for the difference although gender-specific variation has not yet been studied in the U. S. Some theories suggest men might be more affected due to more underlying health conditions than women. Risk factors of heart disease, high blood pressure, and liver disease have historically been more prevalent in men but are now equaling between genders. Males have a higher concentration of angiotensin-converting enzyme 2 (ACE-2) in their blood which makes entry into the cells easier for COVID-19. Women have a longer X chromosome that may improve the immune system. So far, these are theories. The reason for gender differences is unknown.
Medical conditions Many existing medical conditions affect the severity of COVID-19. Most of these medical conditions have immunosuppression and internal body inflammation as consequences of the diseases. These conditions include:
- Cancer
- Chronic kidney disease
- COPD (chronic obstructive pulmonary disease)
- Heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies
- Immunocompromised state (weakened immune system) from solid organ transplant
- Obesity (body mass index [BMI] of 30 kg/m2 or higher but < 40 kg/m2)
- Severe Obesity (BMI ≥ 40 kg/m2)
- Sickle cell disease
- Smoking
- Type 2 diabetes mellitus
- Use of certain medications
- Poverty and crowding
- Certain occupations
- Pregnancy
Some medical conditions may increase the severity of COVID-19. These conditions are under study:
- Asthma (moderate-to-severe)
- Cerebrovascular disease (affects blood vessels and blood supply to the brain)
- Cystic fibrosis
- Hypertension or high blood pressure
- Immunocompromised state (weakened immune system) from blood or bone marrow transplant,
- immune deficiencies, HIV, use of corticosteroids, or use of other immune weakening medicines
- Neurologic conditions, such as dementia (and spinal cord injury)
- Liver disease
- Overweight (BMI > 25 kg/m2, but < 30 kg/m2)
- Pregnancy
- Pulmonary fibrosis (having damaged or scarred lung tissues)
- Thalassemia (a type of blood disorder)
- Type 1 diabetes mellitus
Use of certain medications Routinely taken medications have been noticed to affect the severity of COVID-19. Undocumented information indicates that the supplements melatonin, vitamin D and zinc lessen the severity and course of COVID-19. The anti-reflux drug, famotidine, taken long term prior to contracting COVID-19, seems to produce less effects of COVID-19 symptoms and duration of illness. These supplements and drug should not be randomly taken as they can affect your body, build to toxic levels as with vitamin D, and interact with other medications and foods. Check with your healthcare professional prior to adding or changing medications or supplements.
Medications that increase the progression of COVID-19 have not yet been identified.
Poverty and crowding Individuals who live in poverty are less able to obtain fresh foods and personal protective equipment to reduce their risk of COVID-19. They have less opportunity for healthcare should they become ill. Frequently, this leads to less treatment for underlying conditions as well as urgent/emergency care needs should they develop symptoms. In addition, they may live in crowded housing conditions or with multiple family members in the same dwelling. They are more likely to have occupations that require working in close surroundings with others. The physical setting along with the inability to obtain the supplies needed to reduce risk are often not conducive to avoidance of the disease.
Certain occupations Individuals who must work in crowded conditions or high-density areas are at an increased risk for COVID-19 due to increased exposure. Healthcare workers, essential workers, or any job that involves close contact with other people increases risk.
Pregnancy Pregnant women both develop COVID-19 and are admitted to the ICU and are placed in mechanical ventilation in larger numbers than non-pregnant women. The reason is unclear, but theories suggest it could be due to underlying conditions of older maternal age, a high body mass index and pre-existing diabetes or hypertension. The hypermetabolism of pregnancy could also be a factor.
COVID-19 Risk Factors for Individuals with Spinal Cord Injury
The Autonomic Nervous System (ANS) is affected in spinal cord injury by both trauma and medical conditions. Either the ANS does not effectively send the message that a virus is present or it does not start the immune system to fight the virus or both. The slow response of the ANS can allow any infection to rapidly duplicate and spread.
Immunosuppression is a reduced effectiveness of your body’s response to bacteria and viruses. After SCI, your immune system is not as strong. This is because after a spinal cord injury messages about viruses and bacteria may not be transmitted to the brain for the body to initiate an early or effective response. Individuals who are immunosuppressed are at highest risk for severe cases of COVID-19.
At the time of spinal cord illness or injury, the inflammation process takes over by cushioning the site of injury to try to correct the area where the spinal cord is affected. This is a normal body response to injury. As time passes, the body continues to provide extra fluid to the damaged area of the spinal cord, brain or both as it attempts to correct any injury. This then becomes chronic inflammation. Control of chronic inflammation is difficult as the body has now adapted to a new way of functioning.
The secondary complications of spinal cord injury further compound COVID-19 risk and severity of the disease:
Autonomic Nervous System Dysfunction Spinal cord injury affects the ANS. This is manifested by many issues such as slowing of the cardiovascular system (slow pulse and low blood pressure), decreased vascular response (orthostatic hypotension, increased risk of blood clots), challenges to respiration and cough. The immune response is slowed.
Diabetes is a complication of SCI especially due to lack of movement in the body. Diabetes affects the body’s immune response to all bacteria and viruses.
Heart disease can develop from lack of movement or exercise as well as poor dietary habits or genetics.
Respiratory or urinary tract infection also increase the risk of COVID-19. A poor immune response to an existing infection decreases the body’s ability to fight another infection. A decreased ability to cough or clean debris out of the lungs allows germs to build. Individuals who catheterize are at higher risk of viruses and bacteria because of entry into the sterile urinary system.
Open pressure injuries are another avenue for viruses and bacteria to enter the body. COVID-19 enters the body through mucous membranes. An open injury is a venue for entry for viruses and bacteria.
The spleen is the major infection-fighting organ of the body. If you have a disease that affects your spleen or had trauma to the spleen or removal of the spleen, you have an increased risk of infection.
Pediatric MIS-C
Many children, like adults, have far milder cases of COVID-19 but still require medical attention. Since your child with SCI has immunosuppression, the worst-case scenario of Multisystem Inflammatory Syndrome in Children (MIS-C) associated with COVID-19 can occur. Not every child will have all the symptoms. The diagnosis is made when some or all of these symptoms are present:
- Fever
- Abdominal pain
- Vomiting
- Diarrhea
- Neck pain
- Rash
- Bloodshot eyes
- Feeling extra tired
Seek emergency medical help if your child develops:
- Trouble breathing
- Pain or pressure in the chest that does not go away
- New confusion
- Inability to wake or stay awake
- Bluish lips or face
- Severe abdominal pain
Exposure in children can be up to four weeks prior to symptoms. Your child may have a positive COVID-19 test. The carrier of COVID-19 may or may not show any symptoms. You might not know how the disease was contracted. Anyone in your household who has exposures to the outside world should not have exposure to your child.
If your child has been exposed to COVID-19, they should be isolated and their health professional notified. Protective measures should be continued by washing your hands, isolating, practicing social distancing and reducing number of exposures.
MIS-C has many of the same symptoms as Kawasaki disease so symptoms were not directly linked to COVID-19 right away. Symptoms of Kawasaki disease are fever, rash, swelling of the hands and feet, irritation and redness of the whites of the eyes, swollen lymph glands in the neck, and irritation and inflammation of the mouth, lips, and throat. With either disease, MIS-C or Kawasaki, your child is extremely ill and needs medical attention. Do not delay wondering or trying to sort it out. Call 911.
If you feel your child is in danger, call 911. Do not hesitate. COVID-19 can move rapidly through the body. Emergency care is needed if the child has these symptoms: breathing problems, struggling to breathe, breathlessness that affects talking or movement, confusion, dizziness, sleepiness, fainting, chest pain, cold, sweatiness, pale color, is turning blue or has blotchy skin. Call 911.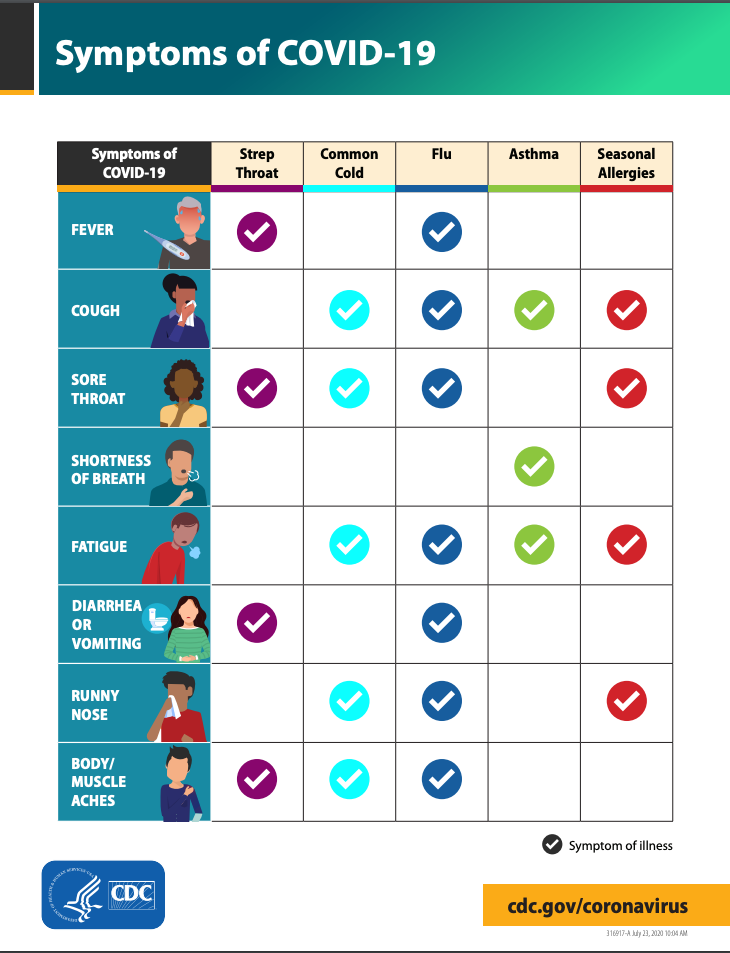
Is It A Cold, Flu or COVID-19?
Symptoms of a cold, flu and COVID-19 overlap. It can be quite confusing. The chart, published by the CDC, can help you determine which you might have. You will only know if you have COVID-19 by testing. Always check with your healthcare professional to make a determination about your health and treatments.
Testing for COVID-19
If you have symptoms or have been near someone with COVID-19, you should call your healthcare provider. They will instruct you where you can get tested. Unless there is an extreme emergency, infected people should not go to healthcare providers’ offices or hospitals to avoid spreading the virus to others. Your medical provider may schedule a telehealth appointment. If you are having difficulty breathing, decreased mental status or another emergency, you should always call 911. Tell them COVID-19 is suspected so the emergency personnel can come prepared to protect themselves and you.
Test kits and testing sites are available. You can order an at-home test kit here, or purchase an at-home test kit at your local pharmacy. In some cases, your insurance may cover the cost of an at-home test kit. The test kit, which consists of a deep nasal swab, or saliva collection test will indicate if you have COVID-19 or not. At-home test kits will give you a result in a few minutes. While a test taken at a testing site can take hours for results. You will need to self-isolate until the results of your test are known.
Antibody tests obtained through a blood sample can indicate if you have antibodies to COVID-19. If you do, you likely have had the virus.
Stay at home in self-isolation if you are sick for any reason. This avoids the spread of COVID-19 as well as other colds and flus. If you have a case of COVID-19 but are being managed at home, stay in your room without visitors. Caregivers may assist you but not linger. If possible, designate a bathroom for your use only.
Vaccines and Treatments for COVID-19
There are two pathways for individuals to either avoid or treat existing COVID-19. Vaccines are used to avoid contracting the virus. Vaccines keep the virus from entering the cells of your body. Vaccines do not eradicate the virus as it still exists in nature. Treatments are being developed to treat the virus once it has entered the body.
Vaccines
Vaccines are designed to stop the viruses from entering cells. For this reason, vaccines work best before a virus enters your body. Vaccines work by imitating a virus. This allows the immune system to develop T cells to neutralize the virus before it can enter your body’s cells. A memory of the specifically developed T cell for a specific virus is kept.
There are five different types of vaccines. Live, attenuated vaccines are an injection of a weakened virus that will not make you sick, inactivated vaccines consist of a dead virus, toxoid vaccines are weakened viruses, subunit vaccines contain only part of the virus, and conjugate vaccines are a different virus but with a coating like the target virus. All stimulate the body to create neutralizing effects.
COVID-19 vaccines are mRNA, viral vector, or protein subunit vaccines.
- mRNA mRNA vaccines use mRNA (created in a lab). Once in your body the mRNA teaches cells to make a protein that triggers an immune response.
- Viral vector Viral vector COVID-19 vaccines consist of a modified version of a different virus (vector virus). This virus will deliver crucial instructions to your cells.
- Protein subunit Protein subunit vaccines are similar to vaccines used for illnesses such as chickenpox. The protein subunit has pieces of the virus that cause COVID-19. Another part of the vaccine contains an adjuvant that aids the immune system respond to the spike protein in COVID-19 in the future.
There are four COVID-19 vaccines in the United States. The U.S. Food and Drug Administration has approved or given Emergency Use Authorization to the following vaccines:
Approved
Pfizer-BioNTech (mRNA)
- Pfizer-BioNTech’s bivalent booster shot is also approved.
Moderna (mRNA)
- Moderna’s bivalent booster shot is also approved.
Emergency Use Authorization
Johnson & Johnson (viral vector)
The FDA has limited the authorized use of this vaccine. The following criteria must be met to qualify for this vaccine.
- Other vaccines aren’t accessible or clinically appropriate.
- Those over the age of 18 who would not otherwise receive a vaccine.
Novavax (protein subunit)
.Thoughts about Vaccines During the first SARS pandemic in the 1970s, the vaccine developed was associated with an increase in the incidence of Guillain Barré, a neurological disease that causes paralysis, typically with some resolution. It was determined there was a defect in the way that vaccine was manufactured. The vaccine development process has long since been changed. Current vaccines are now grown in eggs. You will be asked if you are allergic to eggs prior to taking a vaccine. Talk with your healthcare professional prior to taking any vaccine if you have a history of Guillain Barré or an allergy to eggs.
Recent studies of vaccines show that individuals who have vaccines have less risk of developing Guillain Barré than if you don’t take the vaccine. For instance, your risk of contracting Guillain Barré is less if you have the flu vaccine and greater if you do not have the flu vaccine.
Treatments for COVID-19
Monoclonal Antibodies is a treatment that is thought to reduce the severity and length of time that an individual has COVID-19. These monoclonal antibodies attach to the spikes of the coronavirus which prevents them from entering your body’s cells.
Natural antibodies that are created from individuals who have recovered from COVID-19 are harvested from their blood plasma. They are reproduced in a laboratory and replicated (cloned). Mono means one type. Clonal means cloned or duplicated. Several different monoclonal antibodies might be contained in one treatment.
Monoclonal antibodies are then given by I.V. to a person who has COVID-19 but who is unable to generate enough natural antibodies on their own. This technique for treatment is used extensively in individuals undergoing cancer treatment with few side effects.
The FDA has authorized the use of the following in certain instances:
- Bamlanivimad and etesevimab to be administered together to treat mild to moderate COVID-19 in younger pediatric patients, including newborns.
- Evusheld (Note that as of 1/26/23, Evusheld is not currently authorized for use in the U.S. until further notice by the FDA.)
- Tocilizumab
Antivirals are medications that inhibit viruses from entering the cells of your body. They do not destroy the virus but since it is prevented from entering your body’s cells, it cannot replicate.
Available antiviral medications are:
Oral Antiviral
- Paxlovid
- Lagevrio
IV Antiviral
- Veklury (remdesivir)
You can get these with a prescription from your doctor. Paxlovid can be prescribed by a state-licensed pharmacist.
Hydroxychloroquine and chloroquine are disproven treatments for COVID-19 and should not be used.
Plasma
Individuals who have had COVID-19 and are now well, have antibodies for this specific virus in their blood system because their immune system developed natural antibodies. A transfusion of the donor’s plasma can be infused into a person who has COVID-19 but is not making successful or timely antibodies. This process has boosted the immune system of the individuals receiving the infusion.
Other Medications for COVID-19 Treatment
Serendipitously, some medications that individuals take for other conditions have been related to lessening the course of COVID-19. There is no scientific study of these medications, but anecdotal instances have been reported. Do not initiate taking these medications. Check with your health professional prior to starting any medication or health supplement. Any new medication or supplement can interfere with your regular medication or cause toxic overdosing.
- Aspirin lowers risks of blood clots and reduces inflammation.
- Dexamethasone is an anti-inflammatory and likely reduces the inflammatory effects of COVID-19.
- Oxygen is a medication. Extra oxygen is provided to your body if you cannot take in enough through normal breathing.
- Melatonin is thought to boost the immune system through gaining a good night’s sleep. Whether or not it helps increase your immune system has not been researched.
- Famotidine taken long term for gastric reflux disease (heartburn) before the onset of COVID-19 has been noted it may reduce the need for ICU care and the number of deaths. There is no peer reviewed research. This is anecdotal information.
- Vitamin D boosts the immune system, if you are low in vitamin D. Don’t just randomly take this vitamin. Check with your healthcare professional to see if you have a vitamin D deficiency. Vitamin D can be toxic. It has not been studied if it makes you less susceptible to COVID-19.
- Zinc is suspected to shorten infection time but has not been researched for this purpose.
- Acetaminophen for fever and body aches.
- Antihistamines can decrease congestion and stuffiness.
- Apple cider vinegar for a sore throat.
- Glutathione can help strengthen the immune system.
- Cough medication can aid in thinning mucus.
However, before you take any of these consult with your doctor.
Other Treatments
Treatments provided for individuals with COVID-19 range from home care with medications such as Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) for comfort to hospitalization and intensive care. Treatments are individual to each case.
Mechanical ventilation or assisted breathing using a respirator may be necessary if self-breathing becomes ineffective. This can be temporary or long term. The assistive devices might be CPAP, BiPAP or mechanical ventilation through the mouth or through a tracheostomy (surgical opening).
Dialysis is provided to individuals who have kidney failure. This can be temporary or long term.
Rehabilitation after COVID-19 with SCI
Many individuals who have moderate to severe COVID-19 will require long term rehabilitation therapies. Government restrictions have been eased to allow these survivors access to care in rehabilitation facilities.
Those who might be involved in your care are:
Physiatrist is a physician who specializes in rehabilitation and physical medicine. This person will work directly with you to obtain the therapy and treatments needed for improvement in physical and psychological care.
Internist or General Practitioner is your regular healthcare professional who will follow along with your progress to transition you back to your routine medical care.
Pulmonologist is a medical specialist in respiratory care who can help transition you to breathing on your own or with supplemental breathing equipment as needed.
Respiratory Therapist is a professional who will follow your breathing ability and assist with weaning from assistive breathing devices.
Rehabilitation Registered Nurse assists with integration of new techniques to create independence in your activities of daily living (ADL), medications and treatments.
Physical Therapist assists with gross motor progress including strengthening, balance and movement.
Occupational Therapist assists with fine motor progress including strengthening and activities of daily living.
Speech Therapist will assist in vocalizations and swallowing especially following long term mechanical ventilation or tracheostomy.
Psychologist is extremely helpful for individuals who have had traumatic or chronic health issues. This person can assist you and your family in dealing with re-entry into life.
Dialysis Nurse will assist in long term dialysis or teach you to perform dialysis in your home if you have kidney issues.
Dietician will help you create a diet that you can tolerate with the necessary nutrients to regain your strength and health.
Protecting Yourself from COVID-19
As with any disease or illness, prevention is a good start. For those who are immunosuppressed, such as those with spinal cord injury or have the secondary complications of SCI that can increase your risk of a serious case of COVID-19, there are precautions you can take to reduce your chances of contracting this virus.
Immunizations
Your body needs to be protected from illnesses, especially viruses to keep them from entering your body’s cells. Having an infection, either bacterial or viral will reduce your ability for your immune system to fight COVID-19. Multiple infections challenge your immune system.
Flu shots are important preventions for individuals who are immunocompromised. These provide your body with the immunity needed for the flu strains that are suspected every year. You build an immunity for various flu strains with each flu shot. Flu shots are given one to two times per year. There are two strengths, one is regular strength and the other is a stronger version for elderly or immunocompromised individuals.
Pneumonia vaccination is key to provide protection from the bacteria and viruses that can lead to pneumonia which is common for individuals with spinal cord injury due to ineffective deep breathing and coughing to clear debris from the lungs. The pneumonia vaccination is given every 10 years.
Avoid Using Your Mouth for Functional Assistance
Many individuals with higher level spinal cord injury use their mouths to assist with activities. You will need to stop doing this when outside of your home as the mouth is a major gateway for COVID-19 to enter your body.
Wear a Mask
Use of a mask is necessary if you go outside of your home or personal yard space. Due to immunosuppression, individuals with spinal cord injury, other chronic illness or risk factors are especially vulnerable.
Children under the age of 2 or those with compromised breathing should not wear a mask to ensure breathing is not disrupted. Anyone with compromised breathing should not wear a mask but should practice sheltering in place and social distancing. If your breathing is compromised, the risk of a mask restricting your airflow is great. Rebreathing exhaled air can lead to sleepiness and eventually death. If you are unable to recognize lack of oxygen due to sleepiness or unable to use your hands to remove the mask, the consequences are great.
Children over the age of two without compromised breathing need to have a mask when going out. Children will need to have observation to ensure they are safe with breathing as well as maintaining the position of the mask and to ensure they don’t get it tangled around their neck.
To correctly wear a mask, your nose and mouth must be covered with all sides flush against your skin. Masks with pleats should be worn with the pleats pointing downward. Be sure the ear loops are not so tight as to cause a pressure injury behind your ear or so tight that they pull on your ears causing ear fatigue.
To remove your mask, unfasten the ties or loops around the ears, while holding the very edge of the mask or barely reaching inside the mask. Avoid touching the outside front of the mask because that is where germs may have collected. Gently, pull the mask down, away from your mouth and nose. If the mask is disposable, fold it on itself so the front of the mask is on the inside and throw it away appropriately. Carry a bag with you if there is no garbage receptacle such as when getting into the car. Cloth masks should also be placed in a plastic bag until you can deposit them in the washer for cleaning. Cloth masks should be washed after each use. Disposable masks should be properly discarded after each use.
Handwashing and Face Washing
Clean hands are needed in case you touch your face as they can carry germs, COVID-19 and all other bacteria and viruses to the prime entry points of your body, eyes, nose and mouth. If you catheterize, perform a bowel program or have an open pressure injury, these can also be susceptible entry points.
Be sure to follow strict handwashing rules with great frequency and gusto! Washing your hands is essential to avoid infection. With spinal cord injury, hand washing is essential not only in general but also when doing self-care. Effective hand washing is based on three principles, warm flowing water, soap and friction. Wash your hands for at least 20 seconds to the time it takes to sing Happy Birthday twice. Gloria Gaynor has a wonderful play on her hit, I Will Survive, as she washes her hands. It makes hand washing a lot more fun.
Hand sanitizer works well when you are out. Hand sanitizer works if it contains 60% alcohol per CDC guidelines. 70% alcohol is better. You can make your own wipes by putting wet, soapy paper towels in a tightly sealed bag or food saver box. You will also need a separate wet paper towel set for rinsing and some dry paper towels for drying. Yes, that is a lot to tote around but better than getting a virus.
Due to your wheelchair’s height, you are at a disadvantage because your head is lower than most standing people. This puts you in a vulnerable position. After being out or interacting with others, wash your face as well as your hands. Remember, your face has mucous membranes that allow viruses and bacteria to enter. Wash your hands first then wash your face starting with eye lids, then the rest of your face. Use a clean washcloth each time you wash your face. A face shield, closed at the forehead, can be helpful to protect your eyes. A mask should be worn with the face shield.
Wash or use disinfectant wipes on your wheels and rims prior to coming into your home. Wash what you can, wheel forward or backward and wash the rest of your rims and wheels until you have done all of it. Do the same for canes and walkers. If walking use one set of shoes for going outside that stay outside and that are not used in your home.
Social Distance
Maintain a social distance from others of at least six feet. If you are in a situation where individuals are singing, yelling, cheering or using loud voices, their exhalations can travel further, requiring you to be further away such as 12 to 20 feet or more.
For those who are in a vulnerable position because of their use of alternative equipment for mobility, such as a wheelchair, you are below the respiratory droplets of others. Social distancing is very important to keep out of the field of respiratory exhalation of others. This is a minimum of six feet of distance. Besides washing your hands, wash your face, eyes first with warm water and soap on your face after your hands.
Avoid crowds. This is going to be a challenge for everyone. We like to socialize. Think of other ways to gather. Social media will really come into play now. Don’t forget the old telephone for that vocal contact. Check on your neighbors regardless of age or abilities.
It is fine to go outside in uncrowded areas. Getting some sun and fresh air is appealing to everyone. It only takes a few minutes of sunshine to increase the vitamin D in your body. Do not start any supplements unless it is determined that you have a need for them as some, like vitamin D, can become toxic. Your healthcare provider can determine your need through blood tests. Adding any supplement can conflict with your medication.
Just because opportunities for going out into the world are available, it does not mean it is mandatory that you attend. You might choose to do so but remember to evaluate the risks versus the benefits. The risk of going out with others is COVID-19. The benefit of staying home during the COVID-19 pandemic is health.
Avoid individuals who have been in large groups, who have recently traveled or have exposure to COVID-19 as well as other colds and flus. Recent guidelines suggest groups of less than 50. Scientists suggest even smaller numbers. Some say gatherings should be no larger than ten. One of the most common hot spots for contracting COVID-19 are in small groups, even family groups.
Clean Surfaces COVID-19 mostly spreads by respiratory droplets but these fall and land on surfaces. Keep surfaces clean with sanitizing wipes or soap and water scrubs. This can include wheelchair rims, canes and walkers, other assistive devices, door and car handles, counters, keys, handrails, or any other surface that you could touch.
Gloves
You may choose to wear disposable gloves when out of your home. Some people may use disposable gloves when pushing their chair outside. Just remember not to use your mouth to remove gloves or touch your face while wearing them. Gloves do not provide immunity from washing our hands.
Because many people use gloves incorrectly, they have been thought to spread more disease. People tend to think wearing gloves provides safety, but they only work if you touch one thing and then change the gloves. Also, remember when you have your gloves on, not to contaminate yourself by touching your face, just as you should not touch your face with your bare hands. With spinal cord injury, you also have risks when catheterizing, doing a bowel program or have an open injury such as a pressure injury.
The removal process makes gloves inefficient and promotes a false feeling of invincibility when gloves are on. If you chose to wear gloves, put them on as you would any glove but position your hands down by your waist, away from your face.
When removing your gloves, again, hold your hands down by your waist, away from your face. With your gloved hand, pinch the outside of the glove on one hand close to your inner wrist but don’t touch your skin, only the glove. Pull the glove down and off turning it inside out as you do. Keep the removed glove as a wad in your gloved hand. Then with your naked hand reach inside the top of the remaining glove at the inner wrist and gently slide it down, skimming it off. The first glove will now be inside the second glove which is inside out, acting as a little plastic bag to hold your trash until you can properly dispose of it. Don’t snap the gloves or remove them with a flourish. You want to keep those germs contained. Immediately wash your hands or use hand sanitizer.
Caregivers and Visitors
All visitors should remove their shoes by the door. Upon entering your home, caregivers or visitors should wash their hands thoroughly. Caretakers and visitors, especially those who are not sheltering with you, should wear a mask especially when providing care.
A caregiver should change into clean clothes when entering your home. They can bring freshly washed clothes in a self-sealing bag.
Talk with your caregiver about their life outside of your home. You might need to make different arrangements if they are not cautious in their personal life.
General Health
Drink fluids adhering to your bladder program restrictions or freely if you have no restrictions either for your bladder or other health issues. Water is the best fluid as it hydrates the body, keeping it healthy and well-functioning. Hydration is always important. Due to bladder programs, it can be difficult to take in more water than you are allotted. Do NOT overwhelm your system but try to take just an extra sip of water every hour when awake. This can create an increase in hydration your body needs without much effect on your bladder program.
Eat a well-balanced diet. This also keeps your body in good health and function. Check with a dietician to ensure you are obtaining the right nutrients for your individual needs. There is a lot of information about dietary effects for the immune system. Eating a healthy well-balanced diet is beneficial to everyone. Foods that can help build the immune system include spinach, fresh kale, swiss chard, bell peppers, strawberries and mushrooms. These foods in frozen form have the same benefits. It does take time to build the immune system through diet. One meal is a start, but it takes time to reap the benefits.
Prioritize Exercise
If you do not exercise, now is the time to start with range of motion. Start slow but over time, work up to three times a day. Talk with your healthcare professional about a good exercise program and to ensure you are ready to exercise.
Exercise your body, especially the part that has decreased function. Your body above and below the level of your injury craves movement. This can boost your immune system, improve circulation, decrease contractures and tone (spasms) and improve your mental wellbeing. You could be healthier coming out of the pandemic than when it started.
Sleep Hygiene
A good night’s sleep boosts the body’s immune system. It allows the brain and body time to rest and reprocess itself. Keep the TV and music off so your brain is not disturbed. Do not use electronics for two to four hours before going to bed or in the night. Try to go to bed at the same time and get up at the same time. These habits help to create a better, more restful sleep.
Maintain your Mental Health
Seek to improve or maintain mental wellness. Keep your mind fit as you keep your body fit. This can include increasing your horizons and activities to seeking counseling to improve coping skills, especially while social distancing.
Get involved with people. Talk to others and connect in new ways, on the telephone or computer. Social distancing does not mean social isolation.
If you find the pandemic overwhelming or are having difficulty with sadness, depression, isolation, or other situations, call your healthcare provider for assistance. You can also text the Crisis Text Line at 741741 or call the National Suicide Prevention Lifeline 1-800-273-8255. Boys Town has a toll-free line for callers who are in crisis or are suicidal: 866-697-8394.
Protecting your Respiratory System
Coughing helps to keep your lungs clear of debris such as mucous and particles that enter the lungs as you breathe. Coughing also helps disrupt viruses and bacteria from making a home in your lungs. It won’t completely stop you from becoming ill, but it can help move debris around and out of the lungs. Perform three deep breaths followed by a cough at a minimum of four times a day.
Cover your coughs and sneezes by using a tissue and then immediately discarding it in a trash receptacle. Do not save tissues from one use to another. Wash your hands afterwards. Alternatively, cough into your inner elbow to avoid spreading germs to others. Wash your hands afterwards.
If you have an incentive spirometer from your hospital or rehabilitation stay, now is the time to use it. They can be purchased online. This is a plastic device with typically three balls each in a chamber. Draw air into your lungs while using the mouthpiece to make the balls flow up in the chambers. Try to hold the balls up while breathing in. Start low and build up tolerance. This can help reduce flus and colds by keeping your lungs clear and healthy. Clean your incentive spirometer mouthpiece and tubing with soap and water daily.
Getting Supplies
Everyone needs supplies. Delivery services for products and food are very helpful. Have the package left at the door and bring it in after the delivery. Drive throughs and contactless pickups are helpful as well. Wear your mask. Wash your hands or use hand sanitizer after touching and removing any packaging.
If you do need to go to the store, start at the location where the cart cleaner wipes are. Most stores have you get your cart and then clean it. Once you have touched the cart, you have picked up the germs! Start with the cleaning wipes, wipe your hands with them, use new wipes to clean the pushing bar then use your cart. If you have access to the hand wipes at the exit, re-wipe your hands on the way out.
Inexpensive disposable gloves work great at the grocery store due to handling of products. Do not be lulled into the use of gloves. You cannot touch your face even with gloves on.
Rely on family and friends to help you when outside of your home. Have them shop and run errands if possible.
Stay Positive and Cautious
There are a few things that can help you adjust to this shift in life.
First, get up at a regular time every day. Most people already do this, but it is very easy to snuggle down just a bit longer when you do not have to leave the house. Regular times of getting up and going to bed will help your body and mind. This can also improve your sleep pattern.
Second, get dressed. Change your clothes in the morning to signal to yourself that it is a new day. Occasionally, put on something nice, even if you cannot or choose not to go out.
Third, pay attention to personal hygiene. You might not be going out or seeing people in person, but your general health and mental wellbeing will welcome personal cleanliness.
Structure Your Day
There are several ways to organize your day. Some people who go out daily for activities or work find being at home is like a long weekend or vacation, until they realize there is no return to routine date set. It can become easy to do nothing which will lead to boredom and increase anxiety. Creating a new routine will help with consistency so even though no one can control the outside world, you can control your own personal activities.
Putting some self-imposed structure into your day might be the choice for you. After spinal cord injury, there is some structure that needs to happen such as bladder care, bowel programs and skin care. You already have these built into your day. Without a regular routine, these activities can slide to a point where your routine is no longer followed which can lead to unnecessary complications. Be sure to stick with your daily routine for care even if the usual signals that you use for initiating the activity are not there.
Create a schedule for yourself. Break tasks down into simple steps to be accomplished over days or weeks so you do not become bored or overwhelmed with any one activity. When locked into just one activity, you might forget to catheterize, do your pressure releases or even eat in a timely manner. On the other hand, people who are now in their homes and can choose what and when to do something tend to eat too often, or snack continuously. A schedule for your new environment can help.
Think of things that you would like to accomplish. This might be doing something new that you did not have time to do before. Create a daily routine that includes self-care, work or school. Include activities that are required of you. Then put in your chosen activities. For instance, without leaving your home, you might find you have extra time in the day that you previously used for commuting or you might not be shopping but ordering online or having a neighbor shop for you. Since we are sheltering in place, you might have more time to occupy yourself.
Randomize Your Day
Some individuals do not like structure. You can still organize your day to ensure your health without a strict schedule. You will need to do your routine self-care, work and school but in your free time, choose some activities that you would like to accomplish. Write them on a piece of paper and put them into a bowl. You can draw them out when needed and begin that task. It adds an element of novelty to the day. This approach will make it much more palatable to those who appreciate less rigidity.
Mix Structure and Randomization to Your Day
People generally prefer a little of both structure and randomization, so mix or switch between the two. You are not bound by a strict set of rules, but you do need to live life. The important aspect is to keep working toward tasks or goals, so you have a sense of accomplishment instead of just whiling away the hours. Some sort of plan or structure can help reduce stress in uncertain times.
COVID Research
The effects of COVID-19 are many. The US government studied COVID-19 to assess the long-term effects. This study is called the COVID-19 Observational Study (CORAL). It is being conducted by the National Institutes of Health (NIH) National Heart, Blood and Lung Institute (NHLBI). As an individual with spinal cord injury, if you contract the COVID-19 virus, you might choose to participate in this study as it will be critical to see how those living with SCI are affected.
The CORAL study will help understand long term effects. Incidental reports indicate those who survive COVID-19 may have long term issues with fatigue, shortness of breath, muscle pain, confusion, headaches and hallucinations. Other problems include heart inflammation and muscle wasting, lung inflammation including a chronic dry cough, shortness of breath and pain with breathing. Some individuals will need breathing assistance long term. The nervous system can be affected with headaches, dizziness, trouble concentrating and recall of information. In addition, blood clots are an issue.
Analysis of short- and long-term effects of COVID-19 continue. Some people infected by COVID-19 experience long-term effects (post-COVID conditions, PCC) or long COVID.
Long COVID conditions can last weeks, months or years.
Long COVID isn’t limited to people who experienced severe COVID-19 illness, anyone infected can have post-COVID symptoms.
Those who aren’t vaccinated have a higher risk of post-COVID conditions versus those who are vaccinated.
Sometimes those who didn’t test positive or were asymptomatic can have post-COVID conditions.
The CDC and its collaborators continue to research who experiences post-COVID conditions and if specific groups are at a higher risk than others.
Long COVID Symptoms
General (not limited to these)
- Fatigue or exhaustion that interferes with daily tasks
- Worsening symptoms after physical or mental effort
- Fever
Respiratory and Heart
- Shortness of breath or difficulty breathing
- Chest pain
- Cough
- Heart palpitations
Neurological Symptoms
- Brain fog
- Headache
- Lightheadedness
- Sleep issues
- Pins and needles feeling
- Anxiety or depression
- Change in taste or smell
Digestive Symptoms
- Stomach pain
- Diarrhea
Other Symptoms
- Rash
- Joint or muscle pain
- Issues with menstrual cycle
Clinical Trials and Vaccines
Even though there are FDA approved or emergency use authorized vaccines and booster shots, researchers continue to research for effective ways to prevent or decrease the side effects of COVID-19. Why? Because as COVID-19 mutates it creates variants and subvariants. Some of these subvariants are becoming resistant to vaccines.
To help find effective vaccines and treatments researchers conduct clinical trials. Clinical trials have four stages.
Phase 0 studies include a small number of people. These people are given a few small doses of a new drug. The test could be to see if a drug reaches a tumor, how it affects humans, and how cancer cells in a human body respond to the drug. Phase 0 studies are rare.
Phase I clinical trials are normally the first to involve people, usually 20 to 100. The trail can include individuals living with a condition or disease as well as healthy individuals. This phase helps doctors discover if the drug is safe. During this phase researchers seek the safest and most effective way to administer the drug. Phase I clinical trials can last several months.
Phase II are studies that have passed Phase I. A larger group of participants, often 100-300 people, are involved in this phase. Most phase II trials last from several months up to two years. Participants are put into different groups. One group will receive the standard treatment while the other receives the new treatment.
Phase III trials can have up to 3,000 people enrolled. The enrollees are those with the disease or illness being targeted. Often, when a phase III study begins it starts at the same time at all of the research centers where the trial is being held. Phase III trials are conducted to expand and confirm the effectiveness and safety from the previous phases. Like phase II trials, people are placed in different groups. Unlike phase I or II trials, some participants may be placed in a placebo group. However, a placebo is never used by itself if there is a treatment available that works. This phase lasts one to four years.
Phase IV clinical trials are often referred to as “post marketing surveillance.” A phase IV trial can enroll several thousand people. This phase occurs after the drug is already on the market and available to those who require it. The objective of this phase is to further test for efficacy and safety. Unlike the previous stages, the drug is tested in real life scenarios. The objective is to research the long-term risks and benefits while uncovering potential side effects.
Humanitarian Use is sometimes declared after Phase II trials, rarely after Phase I, for deadly diseases for which there is no other alternative. Some of the treatments in development are being designated for individuals with severe cases of COVID-19 due to lack of treatment options.
Treatments for COVID-19 are being developed by many companies around the world. Some are being developed specifically for COVID-19, others are existing medications that are being repurposed for COVID-19. An example is Favipiravir from Fujifilm Toyama Chemical which is an antiviral developed for prevention and treatment of Ebola virus. It is under study for COVID-19. Another is inhaled nitrous oxide which is under study as it is thought to prevent entry of COVID-19 into cells.
Facts and Figures
For the number of cases of and deaths from COVID-19 in the U.S., see the CDC’s website COVID Data Tracker or Johns Hopkins’ COVID-19 Dashboard.
For the number of cases or deaths from COVID-19 in the world, see the World Health Organization’s COVID-19 Dashboard.
The death rate for pneumonia, influenza and COVID-19 is 7.2%.
About 80% of individuals who contract COVID-19 survive it.
Resources
If you are looking for more information about COVID-19 or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm EST.
Additionally, the Reeve Foundation maintains fact sheets with additional resources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to organizations, including associations which feature news, research support, and resources, national networks of support groups, clinics, and specialty hospitals.
Community Resources:
The Centers for Disease Control and Prevention has the most up to date resources for information about COVID-19. Check this website prior to making decisions about your care or treatment for the latest information. https://www.cdc.gov/coronavirus/2019-nCoV/index.html
Clinical Guideline:
Nicola M, O’Neill N, Sohrabi C, Khan M, Agha M, Agha R. Evidence based management guideline for the COVID-19 pandemic – Review article. Int J Surg. 2020 May;77:206-216. doi: 10.1016/j.ijsu.2020.04.001. Epub 2020 Apr 11. PMID: 32289472; PMCID: PMC7151371. https://pubmed.ncbi.nlm.nih.gov/32289472/
FURTHER READING
References
Ahn DG, Shin HJ, Kim MH, Lee S, Kim HS, Myoung J, Kim BT, Kim SJ. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19). J Microbiol Biotechnol. 2020 Mar 28;30(3):313-324. doi: 10.4014/jmb.2003.03011. PMID: 32238757.
Baj J, Karakuła-Juchnowicz H, Teresiński G, Buszewicz G, Ciesielka M, Sitarz E, Forma A, Karakuła K, Flieger W, Portincasa P, Maciejewski R. COVID-19: Specific and Non-Specific Clinical Manifestations and Symptoms: The Current State of Knowledge. J Clin Med. 2020 Jun 5;9(6):1753. doi: 10.3390/jcm9061753. PMID: 32516940; PMCID: PMC7356953.
Bilbul M, Paparone P, Kim AM, Mutalik S, Ernst CL. Psychopharmacology of COVID-19. Psychosomatics. 2020 Sep-Oct;61(5):411-427. doi: 10.1016/j.psym.2020.05.006. Epub 2020 May 18. PMID: 32425246; PMCID: PMC7232075.
Bischof E, Wolfe J, Klein S. Clinical Trials for COVID-19 Should Include Sex as a Variable. The Journal of Clinical Investigation, 2020;130(7):3350-3352. https://doi.org/10.1172/JCI139306. Retrieved from https://www.jci.org/articles/view/139306.
Centers for Disease Control and Prevention. (2022, August). Estimated COVID-19 Burden. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/burden.html
Chan JF, Yip CC, To KK, Tang TH, Wong SC, Leung KH, Fung AY, Ng AC, Zou Z, Tsoi HW, Choi GK, Tam AR, Cheng VC, Chan KH, Tsang OT, Yuen KY. Improved Molecular Diagnosis of COVID-19 by the Novel, Highly Sensitive and Specific COVID-19-RdRp/Hel Real-Time Reverse Transcription-PCR Assay Validated In Vitro and with Clinical Specimens. J Clin Microbiol. 2020 Apr 23;58(5):e00310-20. doi: 10.1128/JCM.00310-20. PMID: 32132196; PMCID: PMC7180250.
Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J, Farahmandian N, Miresmaeili SM, Bahreini E. A comprehensive review of COVID-19 characteristics. Biol Proced Online. 2020 Aug 4;22:19. doi: 10.1186/s12575-020-00128-2. PMID: 32774178; PMCID: PMC7402395.
Halpin DMG, Singh D, Hadfield RM. Inhaled corticosteroids and COVID-19: a systematic review and clinical perspective. Eur Respir J. 2020 May 7;55(5):2001009. doi: 10.1183/13993003.01009-2020. PMID: 32341100; PMCID: PMC7236828.
Heneka MT, Golenbock D, Latz E, Morgan D, Brown R. Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimers Res Ther. 2020 Jun 4;12(1):69. doi: 10.1186/s13195-020-00640-3. PMID: 32498691; PMCID: PMC7271826.
Huang L, Zhang X, Zhang X, Wei Z, Zhang L, Xu J, Liang P, Xu Y, Zhang C, Xu A. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J Infect. 2020 Jun;80(6):e1-e13. doi: 10.1016/j.jinf.2020.03.006. Epub 2020 Apr 10. PMID: 32283156; PMCID: PMC7194554.
Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstet Gynecol. 2020 Jul;56(1):15-27. doi: 10.1002/uog.22088. PMID: 32430957; PMCID: PMC7276742.
Kannan S, Shaik Syed Ali P, Sheeza A, Hemalatha K. COVID-19 (Novel Coronavirus 2019) – recent trends. Eur Rev Med Pharmacol Sci. 2020 Feb;24(4):2006-2011. doi: 10.26355/eurrev_202002_20378. PMID: 32141569.
Le Bert N, Tan AT, Kunasegaran K, Tham CYL, Hafezi M, Chia A, Chng MHY, Lin M, Tan N, Linster M, Chia WN, Chen MI, Wang LF, Ooi EE, Kalimuddin S, Tambyah PA, Low JG, Tan YJ, Bertoletti A. SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature. 2020 Aug;584(7821):457-462. doi: 10.1038/s41586-020-2550-z. Epub 2020 Jul 15. PMID: 32668444.
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, Bi Z, Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020 May;109(5):531-538. doi: 10.1007/s00392-020-01626-9. Epub 2020 Mar 11. PMID: 32161990; PMCID: PMC7087935.
Li H, Liu Z, Ge J. Scientific research progress of COVID-19/SARS-CoV-2 in the first five months. J Cell Mol Med. 2020 Jun;24(12):6558-6570. doi: 10.1111/jcmm.15364. Epub 2020 May 7. PMID: 32320516; PMCID: PMC7264656.
Liu H, Wang LL, Zhao SJ, Kwak-Kim J, Mor G, Liao AH. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020 Jun;139:103122. doi: 10.1016/j.jri.2020.103122. Epub 2020 Mar 19. PMID: 32244166; PMCID: PMC7156163.
Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020 Jul;38(7):1504-1507. doi: 10.1016/j.ajem.2020.04.048. Epub 2020 Apr 18. PMID: 32317203; PMCID: PMC7165109.
Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020 Jul 1;5(7):831-840. doi: 10.1001/jamacardio.2020.1286. PMID: 32219363.
Mahmoudi S, Rezaei M, Mansouri N, Marjani M, Mansouri D. Immunologic Features in Coronavirus Disease 2019: Functional Exhaustion of T Cells and Cytokine Storm. J Clin Immunol. 2020;40(7):974-976. doi:10.1007/s10875-020-00824-4.
Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020 May 1;318(5):E736-E741. doi: 10.1152/ajpendo.00124.2020. Epub 2020 Mar 31. PMID: 32228322; PMCID: PMC7191633.
Pascarella G, Strumia A, Piliego C, Bruno F, Del Buono R, Costa F, Scarlata S, Agrò FE. COVID-19 diagnosis and management: a comprehensive review. J Intern Med. 2020 Aug;288(2):192-206. doi: 10.1111/joim.13091. Epub 2020 May 13. PMID: 32348588; PMCID: PMC7267177.
Sanchis-Gomar F, Lavie CJ, Perez-Quilis C, Henry BM, Lippi G. Angiotensin-Converting Enzyme 2 and Antihypertensives (Angiotensin Receptor Blockers and Angiotensin-Converting Enzyme Inhibitors) in Coronavirus Disease. 2019 Mayo Clin Proc. June 2020;95(6):1222-1230. https://doi.org/10.1016/j.mayocp.2020.03.026
Shanmugaraj B, Siriwattananon K, Wangkanont K, Phoolcharoen W. Perspectives on monoclonal antibody therapy as potential therapeutic intervention for Coronavirus disease-19 (COVID-19). Asian Pac J Allergy Immunol. 2020 Mar;38(1):10-18. doi: 10.12932/AP-200220-0773. PMID: 32134278.
Tang Y, Liu J, Zhang D, Xu Z, Ji J, Wen C. Cytokine Storm in COVID-19: The Current Evidence and Treatment Strategies. Front Immunol. 2020;11:1708. Published 2020 Jul 10. doi:10.3389/fimmu.2020.01708
Tu YF, Chien CS, Yarmishyn AA, Lin YY, Luo YH, Lin YT, Lai WY, Yang DM, Chou SJ, Yang YP, Wang ML, Chiou SH. A Review of SARS-CoV-2 and the Ongoing Clinical Trials. Int J Mol Sci. 2020 Apr 10;21(7):2657. doi: 10.3390/ijms21072657. PMID: 32290293; PMCID: PMC7177898.
Uday J. Effect of COVID-19 on the Organs. Cureus 2020 Aug 3;12(8):e9540.doi: 10.7759/cureus.9540. PMID: 32905500; PMCID: PMC7470660.
Wollina U, Karadağ AS, Rowland-Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID-19 patients: A review. Dermatol Ther. 2020 May 10:e13549. doi: 10.1111/dth.13549. Epub ahead of print. PMID: 32390279; PMCID: PMC7273098.
Zhou Z, Kang H, Li S, Zhao X. Understanding the neurotropic characteristics of SARS-CoV-2: from neurological manifestations of COVID-19 to potential neurotropic mechanisms. J Neurol. 2020 Aug;267(8):2179-2184. doi: 10.1007/s00415-020-09929-7. Epub 2020 May 26. PMID: 32458193; PMCID: PMC7249973.
Zhou MY, Xie XL, Peng YG, Wu MJ, Deng XZ, Wu Y, Xiong LJ, Shang LH. From SARS to COVID-19: What we have learned about children infected with COVID-19. Int J Infect Dis. 2020 Jul;96:710-714. doi: 10.1016/j.ijid.2020.04.090. Epub 2020 May 7. PMID: 32389849; PMCID: PMC7204709.